By Business Insider Reporter
Malaria remains one of humanity’s most stubborn and deadly diseases, claiming hundreds of thousands of lives each year and disproportionately affecting the African continent.
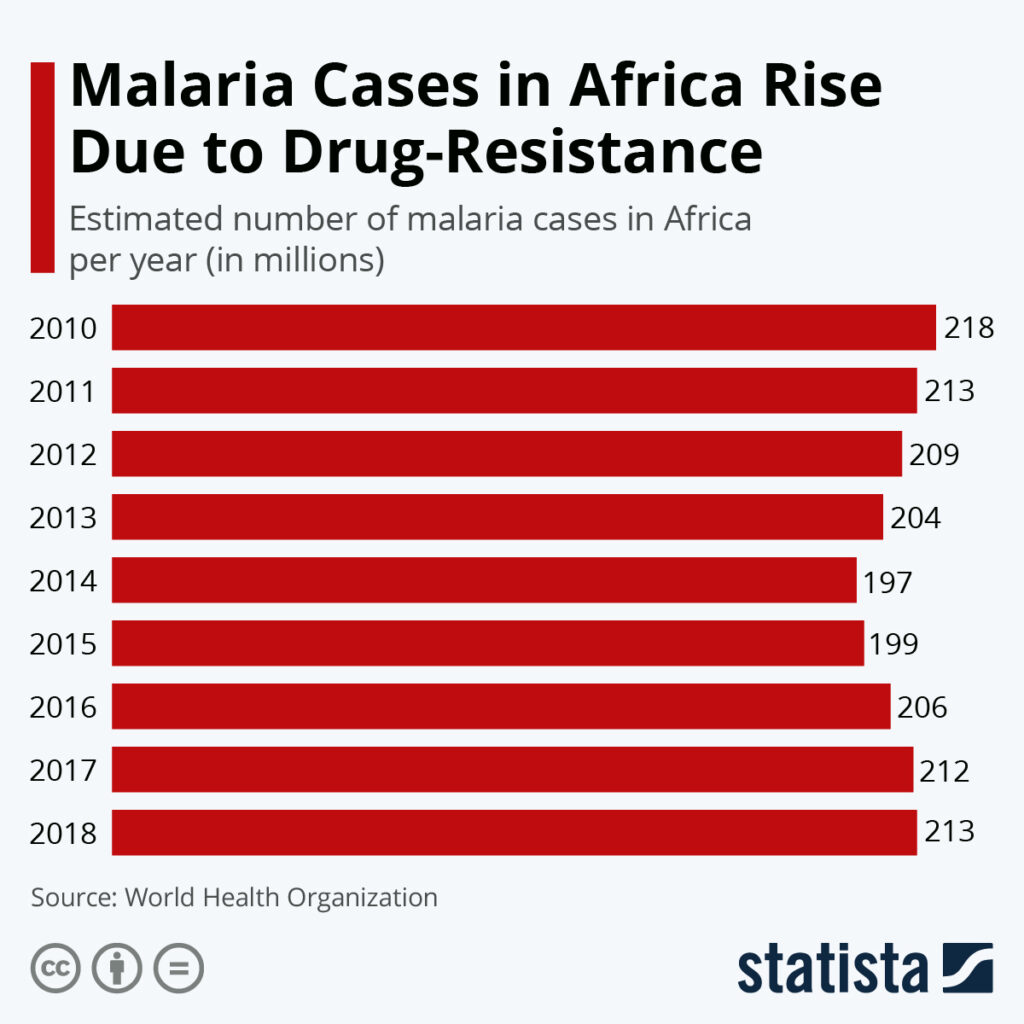
Now, two promising new treatments are offering hope at a critical moment – when drug resistance is rising, health systems are strained, and countries like Tanzania are battling both the medical and economic toll of malaria.
Swiss drugmaker Novartis recently announced that its next-generation antimalarial performed strongly during clinical trials conducted in 12 African countries.
Although the therapy is still at least a year from public release, the results signal the potential arrival of a vital tool in the fight against resistant strains of the parasite. At the same time, researchers in Gabon revealed success with a single-dose combination therapy of four antimalarial medications. In trials, 93 percent of patients were parasite-free within just 28 days.
Together, these breakthroughs come at a pivotal time for Tanzania – a nation that has achieved tremendous progress against malaria in the past decade yet continues to bear a heavy disease burden with steep economic consequences.
The cost of malaria to Tanzania’s economy
Malaria is more than a public-health threat in Tanzania; it is a significant economic brake. The disease disrupts productivity, strains households financially, and consumes government resources.
Estimates from the Ministry of Health and regional development partners suggest that the total economic burden exceeds US$300 million annually, including direct treatment costs and indirect losses from missed work, reduced agricultural output, and school absenteeism.
That comes to nearly TSh 735 billion, a staggering amount in a country where the reality for many families is the constant struggle to put three decent meals on the table.
Malaria accounts for:
- 43 percent of all outpatient visits,
- 35 percent of hospital admissions, and
- A substantial share of childhood mortality.
Such figures make malaria one of the top contributors to underdevelopment in rural communities. Families spend money repeatedly on medicines, transport to clinics, and long recovery periods. Entire sectors – especially agriculture, which is the backbone of Tanzania’s economy – experience productivity losses every rainy season when malaria peaks.

Reducing malaria even modestly has measurable economic benefits. As the World Health Organization has noted, lowering the malaria burden by 90 percent across Africa could boost the continent’s GDP by more than US$16 billion a year. Tanzania stands to gain significantly from such improvements.
National progress: Fewer deaths – but not yet victory
Despite these challenges, Tanzania’s progress over the past decade has been remarkable. National surveys and health facility data show that malaria prevalence has dropped from 14 percent in 2015 to just over 8 percent in recent years.
The number of facility-reported deaths has also fallen significantly – from more than 2,400 deaths in 2020 to roughly 1,500 by 2024, a drop of nearly 40 percent.
Cases remain high, however. Mainland Tanzania still reports 4–4.5 million malaria cases annually, underscoring that while progress is real, the disease remains endemic in many regions, especially in the northwestern and southern parts of the country.
Part of the success stems from expanded access to rapid diagnostic tests, wider use of insecticide-treated nets, and integrated community-based interventions. But the gains remain fragile.
resistance to insecticides is rising, and parasite resistance to frontline drugs – the very problem the new treatments aim to solve – threatens to reverse progress if not addressed quickly.
Major initiatives to fight malaria in Tanzania
Tanzania’s strategy against malaria is broad and increasingly sophisticated, combining traditional prevention with modern genomic and epidemiological tools. Key initiatives include:
Vector surveillance and entomological monitoring
In partnership with WHO and research institutions, Tanzania has built a network of 32 sentinel surveillance sites that monitor mosquito species, density, and insecticide resistance. This data helps guide decisions on which chemicals to use and where to deploy larviciding.
Modern larviciding programmes
Urban centres such as Dar es Salaam, Mwanza, and Tanga have expanded larviciding – targeting mosquito breeding sites with biological agents. Studies show this approach is cost-effective in densely populated environments where mosquitoes breed in predictable locations.
Genomic surveillance of the parasite
Led by the National Institute for Medical Research (NIMR), Tanzania is integrating genomic technology to track mutations in the parasite that could lead to drug resistance. This nationwide programme helps guide treatment policies and ensures early detection of dangerous strains.
The national end malaria council
Formed in 2023, this high-level body brings together government, private sector, civil society, and development partners to pool resources and accelerate action toward the goal of eliminating malaria by 2030.
Increased external funding
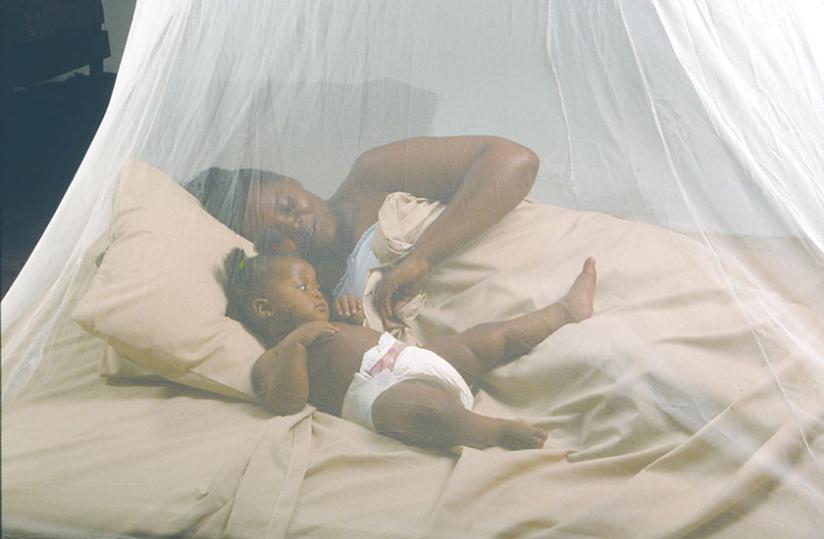
The Global Fund’s US$613 million allocation for 2024–2026 supports universal net distribution, diagnostic supply, and new surveillance capabilities. Long-lasting insecticide-treated nets (LLINs) remain one of the most effective prevention tools for the general population.
Why new treatments matter so much for Tanzania
The emergence of drug-resistant malaria is one of the greatest threats facing East Africa. Tanzania still relies heavily on artemisinin-based combination therapies (ACTs), but resistance has already been documented in multiple neighboring countries. Without effective new drugs, there is a risk of rising treatment failures, longer illness periods, and higher mortality.
The two new therapies announced this year could help fill this gap:
The Novartis treatment
- Designed specifically to combat resistant strains
- Tested across 12 African countries
- Expected to receive regulatory review within a year
The single-dose four-drug therapy from Gabon
- 93 percent parasite clearance within 28 days
- Potential for easier, more consistent patient compliance
- Suitable for rapid deployment in remote areas
For Tanzania, where many rural clinics struggle with medicine stock-outs and patients often cannot return for multi-dose regimens, a single-dose therapy could be transformative.
Turning progress into elimination
Tanzania is at a crossroads. The country has shown strong political commitment, scientific investment, and measurable progress – but malaria remains entrenched in several regions. Climate variability, growing insecticide resistance, and population movement all complicate eradication efforts.
Still, Tanzania’s comprehensive approach provides a strong foundation. Prevention tools are expanding, surveillance is improving, and cross-border collaborations are strengthening. If the new treatments become widely available and affordable, they may become the missing piece needed to accelerate progress.
Achieving elimination by 2030 will require:
- Continued government investment
- Increased domestic resource mobilisation
- Sustained net coverage
- Integration of genomic and digital surveillance
- Rapid rollout of new therapies once approved
The stakes are high. Reducing malaria further would save thousands of Tanzanian lives each year, strengthen the health system, and boost productivity across the economy. For millions of children, it would mean fewer missed school days, better cognitive development, and a brighter future.
Bottomline
With new drug innovations on the horizon and Tanzania’s ongoing public-health efforts gaining momentum, the fight against malaria is entering a hopeful new chapter. The combination of scientific breakthroughs, national commitment, and international support may finally push the country – and the continent – closer to a malaria-free future. For Tanzania, the new treatments are not just scientific milestones. They are potential tools for transformation – tools that could help lift communities out of poverty, strengthen the economy, and save countless lives.